Vaping cessation has emerged as a critical health focus, particularly among teens and young adults grappling with nicotine addiction. This demographic faces unique challenges, as evidenced by a recent study published in JAMA, which highlights the efficacy of varenicline, an FDA-approved smoking cessation pill. Remarkably, those using varenicline exhibited over three times the success rate in quitting vaping compared to individuals relying solely on behavioral counseling. With the popularity of vaping soaring—about a quarter of 18- to 25-year-olds were using them in 2023—effective solutions like varenicline are essential to combatting this growing issue. As we explore various treatment options, the imperative to address adolescent vaping habits becomes clearer, promising healthier futures for those affected.
Addressing the challenge of quitting vaping is imperative in today’s health landscape, particularly for the youth susceptible to nicotine dependence. Alternative solutions, such as the twice-daily varenicline pill, have gained attention due to their significant success rates in helping adolescents and young adults break free from e-cigarette habits. The trend of electronic nicotine delivery systems has surged among teens, necessitating a comprehensive approach to cessation strategies. Research indicates that pharmacological interventions may play a vital role in overcoming the barriers posed by vaping addiction. As we delve into innovative methods to support cessation in this age group, the significance of safe and effective treatments cannot be overstated.
Understanding Vaping Addiction Among Teens
Vaping addiction has emerged as a significant public health concern, particularly among teenagers and young adults. Research shows that about a quarter of individuals aged 18 to 25 reported vaping in 2023, highlighting the pervasive nature of this habit. The allure of vapes lies in their design, which often makes them more attractive to youth compared to traditional cigarettes. Not only are they easy to conceal, but their range of flavors can mask the harshness of nicotine, leading many young users to underestimate the health risks associated with vaping.
The use of nicotine in these products can have serious implications for developing brains. Early exposure to nicotine can predispose youths to stronger addictions to other substances later in life. For this reason, it is crucial for parents, educators, and healthcare providers to understand the dynamics of vaping addiction, including its symptoms and potential consequences. Effective communication about the dangers associated with vaping can lead to better prevention strategies and encourage teens to seek help if they are struggling with addiction.
The Role of Varenicline in Vaping Cessation
Varenicline, an FDA-approved smoking cessation pill, has shown unprecedented effectiveness in helping teens and young adults quit vaping. In a recent study, participants using varenicline had a quitting success rate that was over three times higher than those receiving placebo treatments. This is a significant finding, as it confirms that pharmacological intervention can be effective in addressing nicotine addiction within vulnerable populations. Varenicline acts on the same nicotine receptors in the brain that are activated by nicotine itself, thus alleviating withdrawal symptoms and cravings associated with vaping.
The flexibility of varenicline’s prescription guidelines is also noteworthy; it can be prescribed for individuals as young as 16. With appropriate medical oversight, teenagers seeking to quit vaping can receive the support they need to break free from nicotine dependence. Importantly, the study indicated that the use of varenicline did not lead these young adults to start smoking cigarettes, thereby offering a safe pathway to cessation. Encouraging teens to discuss their vaping habits with healthcare professionals could pave the way for better outcomes in vaping cessation.
Behavioral Support in Vaping Cessation Efforts
While medications like varenicline have proven to be effective in promoting vaping cessation, combining them with behavioral counseling can enhance the overall effectiveness of quitting strategies. In the recent study, participants who received varenicline along with weekly behavioral counseling showed significantly higher success rates compared to their peers who received only behavioral counseling. This indicates that a holistic approach addressing both the physical and psychological aspects of addiction is crucial for developing effective treatment plans for young people.
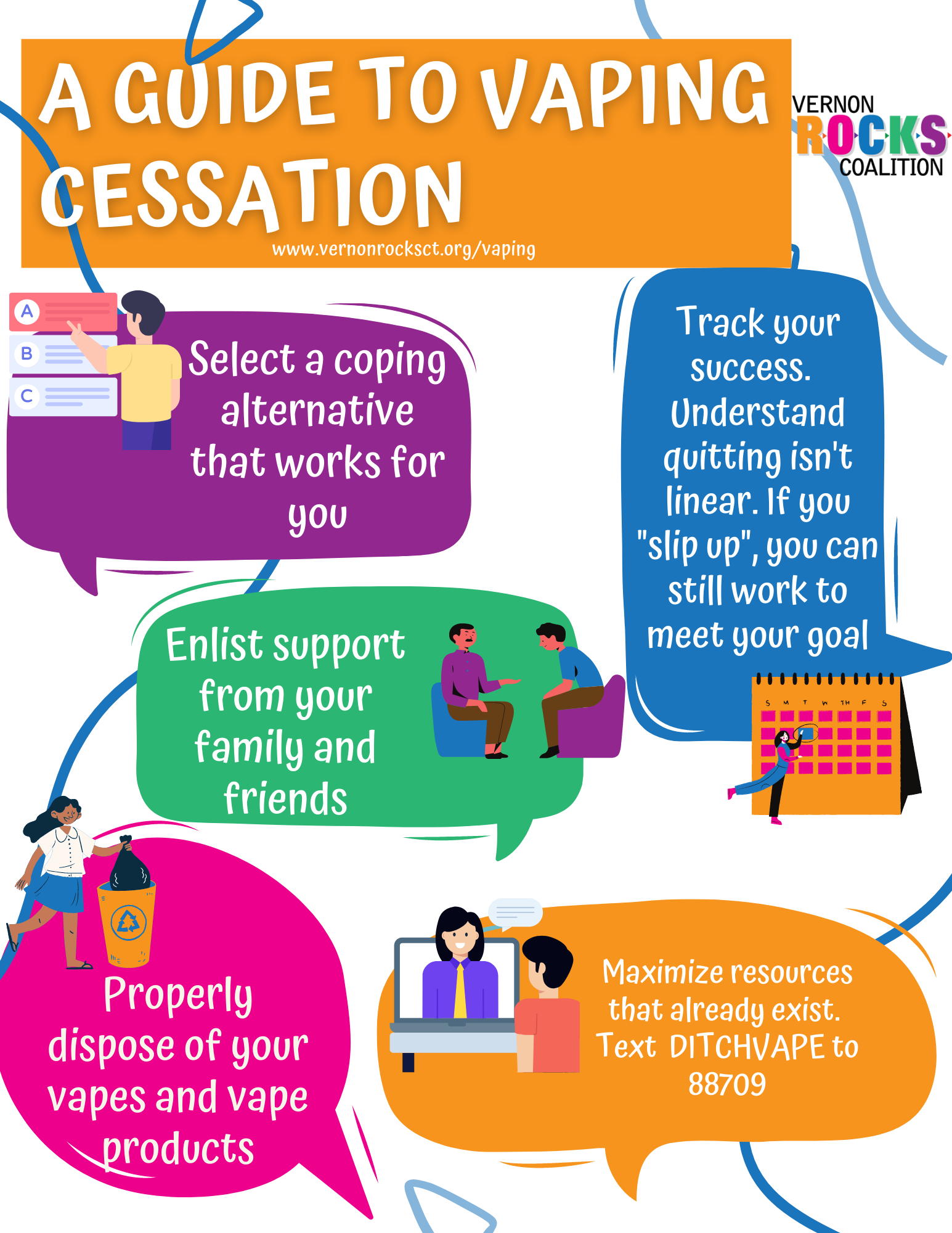
Behavioral counseling provides individuals with coping strategies and support systems that are essential for overcoming addiction. These counseling sessions can help identify triggers and develop personalized plans for avoiding relapse. Incorporating text support services, such as ‘This is Quitting,’ into cessation programs further supplements the efforts by allowing individuals to receive ongoing motivation and guidance. Together, these strategies form a comprehensive support network that can significantly improve the chances of successfully quitting vaping.
The Importance of Early Intervention
Addressing vaping addiction in its early stages is vital for reducing the long-term risks associated with nicotine dependence. Adolescents are particularly susceptible to nicotine addiction, and early intervention strategies can significantly alter the trajectory of their health. Programs that educate youths about the dangers of vaping and provide immediate support can help mitigate the number of new users and prevent existing users from developing severe addiction.
Healthcare systems and educational institutions must collaborate to create environments where teens feel empowered to seek help. The combination of informative initiatives and accessible treatment options, such as the study of varenicline, can effectively address the vaping epidemic among teens. By prioritizing early intervention, we can protect future generations from the health consequences of nicotine addiction.
Health Risks Associated with Vaping
Vaping is often perceived as a safer alternative to smoking; however, it carries its own set of significant health risks. Vapes contain harmful substances, including nicotine, carcinogens, and heavy metals that can lead to severe health issues such as pulmonary inflammation and long-term respiratory problems. For teenagers, the adolescent brain is still developing, making it particularly vulnerable to the effects of nicotine addiction and the subsequent cognitive and behavioral changes that can arise from it.
Research indicates that the exposure to nicotine through vaping can alter brain development, which may lead to increased susceptibility to other addictions in the future. The normalization of vaping among peers can further exacerbate these risks, as it encourages continued usage. Public health campaigns aimed at educating young people about the real dangers of vaping are essential in combating these misconceptions and reducing the prevalence of nicotine dependence in this demographic.
Addressing Misconceptions About Vaping
Many misconceptions exist surrounding the use of vapes, particularly among teens. A common belief is that vaping is entirely harmless or less harmful than smoking traditional cigarettes. However, studies indicate that vaping can lead to serious health issues, including nicotine addiction, which can spiral into more severe health problems over time. It is critical to dispel these myths through accurate public health messaging and educational programs that inform young people about the risks of vaping.
Moreover, the appeal of flavored vapes often clouds the reality of the associated health risks. Young individuals may be drawn to these products due to their flavors, overlooking the fact that they contain potentially dangerous chemicals and addictive substances. By addressing these misconceptions directly in educational settings and community programs, we can better equip teens with the knowledge needed to make informed decisions regarding vaping.
The Future of Vaping Cessation Research
Ongoing research into vaping cessation is crucial for developing effective strategies to combat nicotine addiction among youth. The findings from recent studies surrounding varenicline not only highlight its effectiveness but also signal the need for more comprehensive approaches that may include exploring the effectiveness of combination therapies or new pharmacological options tailored for younger populations. The aim is to create a robust toolbox of treatment methods that can cater to the diverse needs of individuals struggling with vaping addiction.
Moreover, future studies should focus on understanding the long-term impacts of vaping and the transition patterns from vaping to smoking among adolescents. Through this research, public health officials can devise better prevention measures and treatment protocols that protect young users from the adverse health effects associated with vaping. The results of these studies can shape future health policies and ensure that they align with the current trends in teen nicotine usage.
Creating Supportive Environments for Quitting
Establishing a supportive environment is integral in assisting young people in their efforts to quit vaping. This involves not only healthcare providers offering resources but also schools, families, and communities playing proactive roles in supporting cessation efforts. Programs that promote peer support can be particularly effective, as they create safe spaces for adolescents to discuss their struggles and share successful strategies for quitting.
Additionally, schools that incorporate educational programs focused on nicotine addiction and its consequences can empower students with knowledge. Encouraging open dialogues about vaping and mental health creates an atmosphere devoid of stigma, where seeking help is normalized. These supportive environments can significantly enhance the motivation and success rates of teens attempting to quit vaping.
Advocating for Policy Changes to Reduce Vaping
Advocating for policy change is essential in the fight against youth vaping. Policymakers must focus on regulating the marketing and sale of vaping products, particularly those targeting teens and young adults. Implementing stricter age verification processes and limiting flavored products can significantly reduce their appeal and accessibility to minors, thus lowering the rates of initiation among this vulnerable group.
Additionally, public health campaigns that inform the wider community about the dangers of vaping and the need for supportive policies can galvanize public support for change. Working alongside public health organizations, communities can advocate for legislation that promotes healthy living and protects young individuals from the perils of nicotine addiction. These collective efforts can create a safer environment for future generations.
Frequently Asked Questions
How can varenicline help teens vaping quit?
Varenicline, an FDA-approved smoking cessation pill, has been found to be highly effective for teens and young adults wanting to quit vaping. A recent study indicated that those aged 16 to 25 using varenicline were more than three times as likely to successfully quit compared to those who only received behavioral counseling.
What is the success rate of using varenicline for vaping cessation among young adults?
In a clinical trial, 51% of participants aged 16 to 25 using varenicline successfully quit vaping after 12 weeks. This rate significantly surpassed the 14% success rate observed in the placebo group, illustrating the effectiveness of varenicline for vaping cessation.
Are there any risks associated with taking varenicline for vaping cessation?
Varenicline has been shown to be safe for teens and young adults. The study confirmed that participants who quit vaping using varenicline did not turn to cigarette smoking, indicating that it is a viable option for those struggling with nicotine addiction.
What are alternative methods for quit vaping aside from varenicline?
While varenicline has demonstrated significant success in helping teens quit vaping, behavioral counseling and support services like ‘This is Quitting’ are also effective. These methods can be used in conjunction with medication to boost chances of quitting.
What are the dangers of teens vaping and how can cessation help?
Teens vaping can lead to nicotine addiction and heightened risks for addiction to other substances. Quitting vaping with the aid of medications like varenicline can reduce these risks and promote healthier choices among young individuals.
Is varenicline suitable for anyone looking to quit vaping?
Varenicline is specifically approved for adults but can be prescribed for individuals aged 16 to 25 looking to quit vaping. It is important for those interested to consult with a healthcare provider to determine the best cessation plan.
How does behavior therapy complement varenicline for vaping cessation?
Behavior therapy complements varenicline by providing support and strategies to manage cravings and triggers associated with vaping. When combined, these approaches significantly enhance the likelihood of successfully quitting.
What should I know before starting varenicline for vaping cessation?
Before starting varenicline, it’s important to discuss your medical history and any existing conditions with a healthcare professional. Additionally, be prepared for weekly follow-ups to track your progress and success in quitting vaping.
Can younger teens access treatment for vaping cessation?
Currently, varenicline can be prescribed for individuals aged 16 and older. Ongoing research may lead to expanded treatment options for younger teens in the future, highlighting the need for effective cessation strategies.
What role do public health initiatives play in addressing teen vaping?
Public health initiatives aim to raise awareness about the dangers of vaping and provide access to effective cessation resources like varenicline. These efforts are crucial in helping adolescents overcome nicotine addiction and reduce overall vaping rates.
| Key Point | Details |
|---|---|
| Clinical Trial | A study published in JAMA shows varenicline significantly aids in vaping cessation among teens and young adults. |
| Success Rate | 51% of participants using varenicline stopped vaping after 12 weeks compared to 14% of those on placebo. |
| Approval for Ages 16-25 | Varenicline is FDA approved for adults, now also prescribed for 16 to 25-year-olds to quit vaping. |
| Health Risks of Vaping | Vaping exposes users to nicotine addiction and increased risk of drugs like cocaine. |
| Behavioral Support | Participants received behavioral counseling alongside medication to aid cessation. |
Summary
Vaping cessation has seen promising advancements with the use of varenicline, an FDA-approved medication. This study demonstrates that young individuals utilizing varenicline were significantly more likely to quit vaping than those receiving only behavioral counseling. As vaping continues to pose serious health risks among adolescents, effective cessation methods like varenicline are crucial in combating this public health issue.