Brain cancer prediction has emerged as a critical focus in improving outcomes for young patients, particularly those battling pediatric brain cancer. Recent advancements in artificial intelligence (AI) are revolutionizing the way we assess the risk of glioma recurrence in children who have undergone treatment. A groundbreaking study from Mass General Brigham demonstrates how AI can analyze sequential brain scans over time, providing a level of accuracy in predicting relapse risk far superior to traditional methods. By deploying innovative techniques like temporal learning AI, researchers are enhancing the precision of childhood cancer treatment strategies. This forward-thinking approach not only alleviates the burden of frequent imaging for families but also paves the way for personalized treatment plans that target the highest risk patients more effectively.
The landscape of neuro-oncology is undergoing transformation as we delve into predictive analytics for brain tumors, especially those affecting the pediatric population. The utilization of machine learning algorithms is becoming increasingly relevant in assessing the likelihood of glioma recurrence in young patients post-surgery. Innovative methods, such as sequential imaging analysis, are on the rise, offering insights previously unattainable through conventional evaluation processes. By harnessing the power of AI in cancer care, healthcare professionals are now better equipped to tailor treatment pathways, thereby improving the overall management of childhood cancers. This approach not only aims to enhance survival rates but also seeks to minimize the emotional and physical toll on patients and their families.
Understanding Pediatric Brain Cancer
Pediatric brain cancer encompasses various types of tumors that can occur in children, the most common being gliomas. These tumors arise from the glial cells and can significantly impact a child’s development and quality of life. Traditionally, diagnosing and treating pediatric brain cancer involved extensive imaging and regular follow-up scans, as determining the likelihood of recurrence can be challenging. Advances in medical technology are revolutionizing how these cancers are detected and managed.
Moreover, treatment plans often depend on numerous factors, including the tumor’s grade, location, and the child’s overall health. Children with lower-grade gliomas often face treatment strategies that may focus on surgery alone, but for those with high-risk factors, ongoing surveillance and potentially aggressive treatment regimens are required. Hence, early and accurate detection is critical in improving outcomes and minimizing long-term health impacts.
The Role of AI in Pediatric Cancer Care
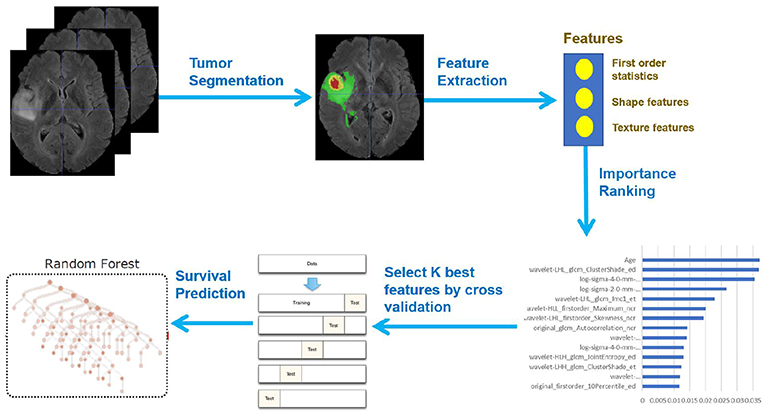
Artificial Intelligence (AI) is transforming how we approach cancer care, particularly pediatric brain cancer, by providing innovative solutions for early detection and treatment optimization. Researchers have developed AI tools that analyze patient imaging data, allowing for a more precise assessment of tumor dynamics over time. This not only enhances the accuracy of predicting glioma recurrence but also aids in personalizing treatment strategies tailored to individual patient needs.
Incorporating AI into pediatric oncology opens avenues for risk stratification, ultimately leading to improved care pathways. The AI models’ ability to synthesize information from multiple MRI scans enables healthcare providers to stay ahead of the disease’s progression and make informed decisions earlier in the treatment process.
Challenges in Predicting Glioma Recurrence
Predicting glioma recurrence remains a complex challenge due to the variable nature of pediatric brain tumors. While many children can be successfully treated with surgery, the likelihood of recurrence can differ significantly. Factors such as tumor grade and post-operative pathology play crucial roles in assessing the risk of relapse, making it imperative for clinicians to utilize advanced predictive tools.
The study highlighted how traditional predictive methods often fall short, with accuracies akin to chance. In contrast, using temporal learning AI technology marks a significant advancement, where AI analyzes multiple imaging events, improving predictive capabilities for glioma recurrence. This innovative approach could transform clinical practice by identifying high-risk patients who may benefit from more aggressive follow-up or treatment.
The Promise of Temporal Learning in AI
Temporal learning is a groundbreaking method that enhances AI’s analytical capabilities by examining sequences of imaging data over time. This technique involves systematically organizing patient scans chronologically, allowing the model to recognize subtle changes that may indicate tumor progression or recurrence. Such a robust framework significantly increases the predictive accuracy compared to analyzing single images.
By utilizing a temporal learning approach, researchers found improvements in relapse prediction for both low and high-grade gliomas, achieving accuracies ranging from 75% to 89%. This stability in predictions not only helps in the management of treatment plans but also in alleviating the emotional and psychological stress on patients and families traditionally associated with frequent imaging.
Advancing Early Detection Tools for Childhood Cancer Treatment
The integration of AI tools in pediatric oncology signifies a significant leap towards more effective early detection strategies. With AI’s ability to analyze longitudinal imaging data, healthcare providers can identify high-risk patients sooner, updating their assessments based on real-time data. This proactive approach can lead to timely intervention, thereby improving overall survival rates and minimizing unnecessary treatments.
Studies have shown that by adopting AI-driven predictive models, clinicians can develop more tailored treatment options. For instance, by accurately identifying children at lower risk for recurrence, healthcare providers might reduce the frequency of follow-up scans, allowing families to focus on recovery without the added stress of frequent hospital visits.
Clinical Applications of AI in Pediatric Brain Cancer
As research on AI’s capability in predicting brain cancer recurrence progresses, the clinical applications appear promising. The ultimate goal is to conduct trials leveraging these AI-driven insights to assess their effectiveness in real-world settings. These collaborations among leading medical institutions are crucial to validate AI methods and integrate them into standard clinical care.
If proven effective, AI tools may not only refine follow-up schedules but also influence therapeutic decisions for pediatric patients. This could transform how childhood cancers are managed, leading to more personalized care that prioritizes the patient’s wellbeing while ensuring that interventions are administered at the optimal times.
Future Directions in Pediatric Brain Cancer Research
The future of pediatric brain cancer treatment appears bright as advancements in AI continue to unfold. With ongoing research focusing on refining these algorithms, the aim is to expand the types of tumors that can be effectively analyzed. Future studies may also delve into integrating genetic and molecular data with imaging, further enhancing prediction capabilities for relapse and aiding in the development of novel treatment strategies.
Moreover, the continued collaboration of institutions and research organizations is vital in pooling resources and information, which can advance knowledge and therapeutic options for pediatric brain cancer. The promise held by AI in revolutionizing cancer care showcases the potential impact on improving survival rates and quality of life for young patients.
The Impact of AI on Pediatric Oncology Care
AI’s introduction into pediatric oncology represents a paradigm shift. Enhanced capabilities in analyzing imaging data can facilitate earlier and more accurate identification of potential health concerns, ultimately leading to more effective patient care protocols. For young patients and their families, the application of these innovations can reduce the uncertainty and stress commonly associated with childhood cancer treatment.
Furthermore, the easing of burdens related to frequent imaging through AI-assisted evaluations underscores a careful balance between vigilance and quality of life. Parents can feel more secure knowing that their child is receiving state-of-the-art care that is at the cutting edge of technology.
Collaborative Efforts in Pediatric Brain Cancer Research
Collaboration is key to advancing research in pediatric brain cancer. By fostering partnerships among major medical institutions, researchers can pool expertise and resources, leading to more effective studies. These partnerships can expedite the validation of AI applications in predicting glioma recurrence, ensuring that groundbreaking discoveries make their way into clinical practice.
Moreover, collaborative efforts extend beyond local institutions, embracing national and international networks which can broaden the scope of research. These alliances pave the way for comprehensive studies that include diverse patient populations, enhancing the generalizability and impact of the findings on childhood cancer care.
Ethical Considerations in AI Usage for Pediatric Cancer
As we integrate AI into pediatric oncology, ethical considerations must also be paramount. Issues related to data privacy, algorithmic bias, and equity in access to advanced technologies must be addressed critically. Ensuring that AI tools are developed and implemented in a manner that prioritizes patient safety and fairness is crucial in maintaining trust within the medical community and the public.
Additionally, as AI’s role in diagnosis and treatment planning grows, continuous evaluation of these tools’ impact on clinical outcomes is essential. Ensuring transparency in how AI models function and the decisions they influence will create a more informed patient experience while reinforcing the importance of human oversight in medical decision-making.
Frequently Asked Questions
What advancements are being made in brain cancer prediction for pediatric patients?
Recent advancements in brain cancer prediction for pediatric patients focus on utilizing artificial intelligence (AI) tools to analyze multiple brain scans over time. A study by researchers at Mass General Brigham showed that an AI model employing temporal learning can significantly better predict relapse risks in children with brain tumors, such as gliomas, compared to traditional methods. This innovative approach enhances the accuracy of recurrence predictions, potentially improving treatment and care for affected children.
How does AI in cancer care improve the prediction of glioma recurrence in children?
AI in cancer care improves the prediction of glioma recurrence in pediatric patients by using temporal learning techniques. By analyzing multiple MR scans taken over time, the AI model identifies subtle changes indicative of potential relapse. This dynamic analysis offers a much higher accuracy—between 75-89%—compared to the approximate 50% accuracy achieved using single images, thus providing crucial insights for better patient management.
What role does temporal learning AI play in predicting childhood brain cancer relapse?
Temporal learning AI plays a pivotal role in predicting childhood brain cancer relapse by synthesizing information from sequentially ordered MR scans. This model captures changes in the tumor’s characteristics over time, allowing for more accurate risk assessments of glioma recurrence. By understanding the progression of the disease, healthcare providers can make more informed decisions regarding follow-up care and treatment strategies.
Why is it challenging to predict recurrence of pediatric brain cancers like gliomas?
Predicting the recurrence of pediatric brain cancers, particularly gliomas, is challenging due to the variable nature of these tumors. While many are treatable, their risk of relapse can differ significantly among patients. Traditional methods often rely on single imaging studies, making it difficult to detect subtle changes over time, which are crucial for accurate predictions. Thus, advanced AI tools are essential in enhancing prediction accuracy.
What potential impact does better brain cancer prediction have on childhood cancer treatment?
Better brain cancer prediction, particularly through AI advancements, can significantly impact childhood cancer treatment by enabling more personalized care. Accurate prediction of glioma recurrence allows for tailored monitoring protocols, potentially reducing unnecessary imaging frequency for low-risk patients. Furthermore, it facilitates timely intervention for high-risk individuals, improving overall treatment outcomes and alleviating stress for patients and their families.
Can AI technology be trusted for pediatric brain cancer predictions?
AI technology, particularly when enhanced with temporal learning methods, has shown promising results in making more accurate predictions for pediatric brain cancer relapse. The study conducted at Mass General Brigham demonstrated a substantial improvement in predicting glioma recurrence compared to traditional techniques. However, further validation and clinical trials are necessary to establish trust in its efficacy and safety before widespread clinical application.
What measures are being taken to validate the accuracy of AI in brain cancer prediction?
To validate the accuracy of AI in brain cancer prediction, researchers are conducting extensive studies that include analyzing nearly 4,000 MR scans from pediatric patients. They aim to confirm the AI model’s effectiveness across various clinical settings before applying it in practice. Future initiatives will include clinical trials designed to evaluate whether AI-informed predictions can enhance treatment protocols for pediatric glioma patients.
| Key Point | Details |
|---|---|
| AI Prediction Accuracy | AI tool predicts risk of relapse in pediatric brain cancer with 75-89% accuracy, compared to about 50% with traditional methods. |
| Temporal Learning Technique | AI uses temporal learning to analyze multiple MR scans over time, improving prediction by recognizing subtle changes. |
| Clinical Implications | Potential to reduce unnecessary imaging for low-risk patients and pre-treat high-risk patients with targeted therapies. |
| Research Support | Study funded by the National Institutes of Health, involved nearly 4,000 MR scans from 715 pediatric patients. |
| Future Directions | Further validation needed; potential for clinical trials to assess AI risk predictions efficacy. |
Summary
Brain cancer prediction has significantly advanced with the introduction of an innovative AI tool that outperforms traditional methods in predicting relapse risk for pediatric patients. This study highlights the importance of leveraging technology, particularly through temporal learning, to improve the accuracy of diagnoses and enhance patient care. As we continue to explore these new frontiers in medicine, the potential to transform treatment strategies for brain cancer patients is promising.